
Niger J Paed 2014; 41 (4): 386 - 389
CASE
REPORT
Eseigbe EE
Diagnostic challenges and
Nuhu FT
Sheikh TL
psychosocial impacts of hypersom-
Oguizu OJ
nia in a Nigerian adolescent: A case
Ezebuiro OGC
report
Eseigbe P
Sanni KA
Baduku TS
DOI:http://dx.doi.org/10.4314/njp.v41i4,19
Accepted: 3rd May 2014
Abstract Hypersomnia,
a disorder
intelligence
was
also
normal.
of
sleep characterized by exces-
There was no contributory past
Eseigbe EE (
)
sive quantity of sleep and exces-
medical history or demonstrable
Eseigbe P
etiology.
Magnetic
Resonance
Departments of Paediatrics &
sive daytime sleepiness (EDS),
Family Medicine,
could adversely affect health out-
Imaging (MRI) of the brain, Elec-
Ahmadu Bello University Teaching
comes in childhood. To highlight
tro Encephalogram (EEG), assay
Hospital, Shika Zaria, Nigeria
diagnostic challenges and the im-
of
serum electrolytes were all nor-
Email: eeeseigbe@yahoo.com
pact of childhood hypersomnia in
mal while screening test for try-
a
resource limited setting, a 14
panosomiasis was negative. Poor
Nuhu FT, Sheikh TL, Oguizu OJ
year old Nigerian who presented
level of awareness, high cost of
Sanni KA
with a seven year history of hy-
evaluation and limited facilities for
Federal NeuroPsychiatric Hospital,
persomnia was studied. Screening
diagnosis of sleep disorder were
Kaduna, Nigeria
for sleep disorder using BEARS
the major diagnostic challenges.
Ezebuiro OGC
sleep algorithm and assessment
Depression, poor academic per-
Nigerian Institute for Trypanosomiasis
for
EDS
using
the
Epworth
formance, suicidal ideation and
Research, Kaduna, Nigeria
Sleepiness Scale were both posi-
stigmatization were all associated
tive for EDS. The assessment of
with hypersomnia in the patient.
Baduku TS
sleep hygiene using the Adoles-
Department of Radiology,
cent Sleep Hygiene Scale was
Keywords: Hypersomnia,
adoles-
Kaduna State University, Nigeria
normal and the use of Ravenís
cence, depression, sleep disorders,
Progressive Matrices to assess
d
iagnostic challenges
Introduction
prevalence of sleep disorders in the Nigerian population
are lacking . However studies on EDS, the cardinal fea-
7
Sleep disorders such as hypersomnias, parasomnias, and
ture of hypersomnia, from Nigeria indicate a prevalence
insomnias could impair development and result in poor
of
53% among children with neurological disorders,
health and social outcomes in childhood . Hypersom-
1,2
44.8% among adults with depression and 17% in a
school population . An EDS prevalence rate of 15%
7-9
nias, characterized by an excessive quantity of sleep and
excessive daytime sleepiness (EDS), is one of the major
has also been reported from a school population in the
categories of sleep disorders identified by the Interna-
United States while worldwide estimates put the preva-
tional Classification of Sleep Disorders (ICSD-2) .
3-5
lence of EDS as ranging four to 30% in adult popula-
tions .
3,6
Sleep disorders in this category include narcolepsy and
its variants, idiopathic hypersomnia with and without
long sleep time, behaviorally induced insufficient sleep
In
adolescence the recommended sleep duration is 8.5 to
10.5 hours daily . However self-reported nocturnal
10
syndrome, and recurrent hypersomnia typified by Klein-
Levin syndrome . Also in this category is hypersomnia
4,5
sleep time declines across the adolescent span just as
bed times grow later and rising times earlier . In addi-
10
due
to substance abuse and medical conditions, such as
obesity, obstructive sleep apnea, depression, head
tion
adolescents have a higher tendency for daytime
trauma and brain tumors .
4,5
sleepiness which is not related to the amount of sleep at
night . Thus incidence of hypersomnia is susceptible to
10
The estimated prevalence rates for the hypersomnias
inappropriate estimation in adolescence. Nevertheless,
include: 0.3% for idiopathic hypersomnia, 0.045% for
hypersomnia has ominous implications for cognitive
narcolepsy and a range of 1-4% for the behaviorally
development with impairment in learning, motivation,
attention span and academic achievement
1,2,11
induced insufficient sleep syndrome . Studies on the
6
.
Further-
387
more
its incidence in adolescence has been associated
(SMR) staging was Stage 3 (Mid- Adolescence). The
with
increased susceptibility to accidents, and depres-
initial screening assessment for sleep using BEARS
sion
3,12
. It
could also signify presence of a grave medical
sleep screening algorithm indicated that EDS was the
only
affected domain. The Adolescent Sleep Hygiene
13
condition such as a brain tumor . Consequently child-
6
hood
hypersomnia demands comprehensive assessment
Scale (ASHS) score was 63% of the maximum score
and indicative of normal sleep hygiene.
14
and management.
The Epworth
Studies and reports on childhood sleep and sleep related
Sleepiness Scale (ESS) score was 19 (Table 1), with
disorders, particularly in an environment like ours with
maximal scores in all sedentary parameters, indicating
EDS
7,15
limited services for sleep disorders, could increase
.
The examination of the central nervous system
awareness and facilitate the development and provision
was normal except for the findings of: loss of interest,
of
such services . The studies could achieve these
7,8
sad mood, impaired concentration and suicidal ideation
through increasing awareness, and providing data, on
while using the Hospital Anxiety and Depression Scale
(HADS) instrument to assess for depression . His
16
the
need to provide diagnostic and therapeutic services
for sleep disorders.
HADS score was 12 which is greater than the cutoff for
depression. Assessment of intelligence using the Ra-
To
promote awareness and highlight diagnostic chal-
venís Progressive Matrices indicated an average intel-
lenges
as well as the impact of sleep disorders in child-
lectual
capacity and performance. The Card Agglutina-
hood
in our environment we studied a 14 year old who
tion Test for Trypanosomiasis (CATT) was negative.
presented with hypersomnia of unknown etiology. It was
The Electro Encephalo Gram (EEG) and serum electro-
the
first of such a case in the first 3000 cases seen at the
lytes and urea assay showed no abnormality. The Mag-
Child and Adolescent Mental Health (CAMH) Unit of
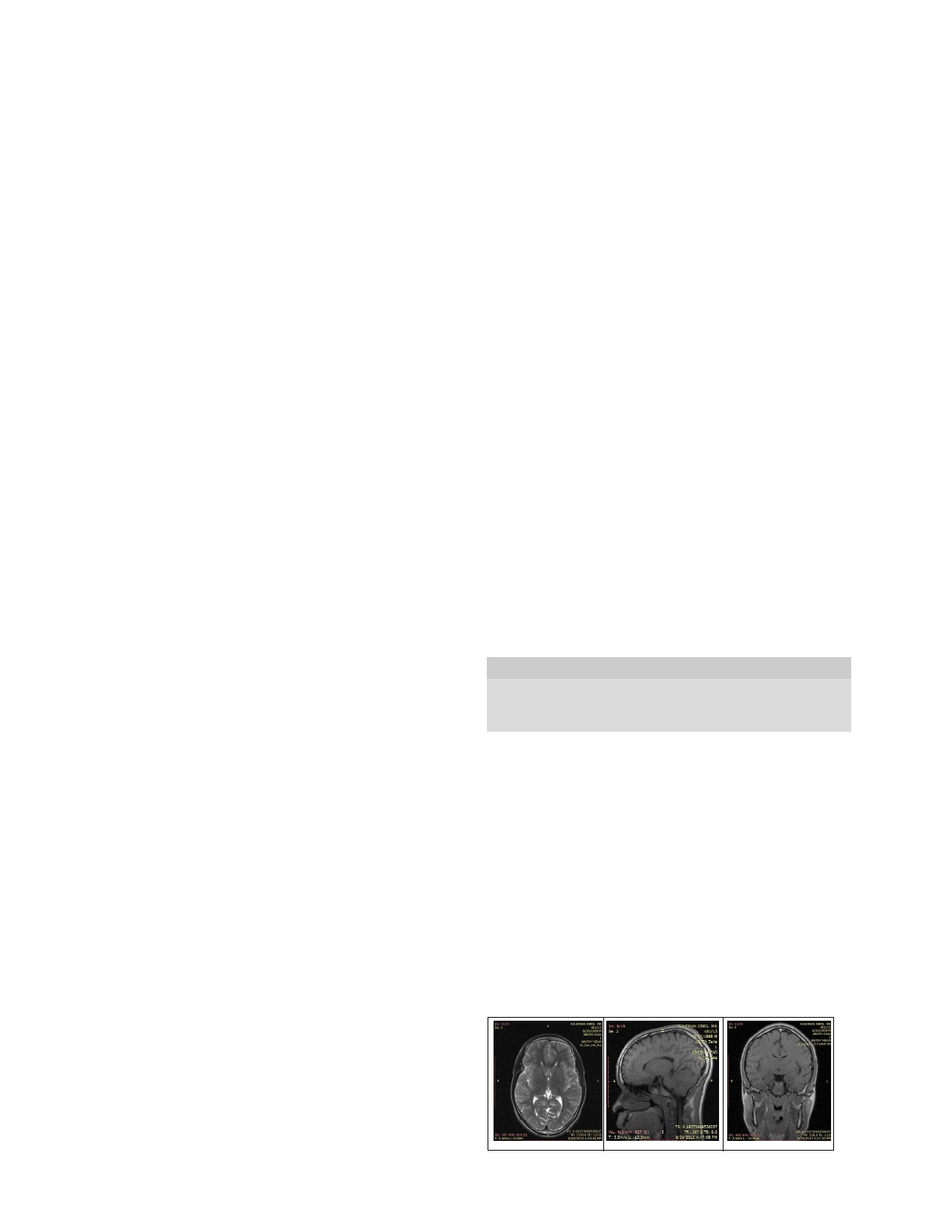
netic Resonance Image (MRI) scan of the brain (Fig 1)
the
Federal Neuro Psychiatric Hospital (FNPH) in
showed mild prominence of the sulci which was re-
Kaduna, Northern Nigeria.
ported as a normal variation. In the absence of structural
abnormalities and considering the fact that childhood
Case Report
peaks of gray matter development is followed by a de-
cline in adolescence, the MRI was reviewed as normal
by
the authors . Due to lack of facilities for sleep stud-
17
S.J. is a 14 year old male who presented to the CAMH
Unit with a seven year history of excessive sleep during
ies in the CAMH unit and in our region of practice poly-
the day. The informants were the patient and his parents.
somnography and multiple sleep latency test (MSLT)
In
the 18 months prior to presentation the duration of his
were not done. Despite subsidization the estimated cost
day time sleep had increased to an average of 45 min-
of
the investigations was a hundred thousand naira ($
utes with a frequency of 4 times daily. His sleep at night
625.00) as against the eighty thousand naira ($500) av-
was described as normal lasting an average of eight0
erage monthly income of the family.
hours per night. There was no history of sleep related
Table 1: Patientís
Epworth Sleepiness
Scale (ESS)
8,15
hallucination, weakness, snoring or that suggestive of
score
difficulty with breathing while at sleep. The patient was
Activity
Situation Chance
not on any routine medication nor was there a history of
of
Dozing (Score
substance abuse. There was no past history of trauma to
0-3)*
the
head, that which was suggestive of meningitis or
1
Sitting and reading
2
encephalitis. The patientís EDS was initially attributed
2
Watching TV
2
to
laziness by parents and school teachers. However
3
Sitting, inactive in a public place (e.g. a
3
progression in the duration and frequency EDS necessi-
theatre or a meeting)
4
As
a passenger in a car for an hour without
3
tated several visits to the family clinic and other secon-
a
break
dary health facilities where parents were reassured the
5
Lying down to rest in the afternoon when
3
patient would overcome his sleepiness. His growth is
circumstances permit
said to be normal and comparable to that of his siblings
6
Sitting and talking to someone
1
7
Sitting quietly after a lunch without alcohol
3
and peers. His academic performance was described as
8
In
a car, while stopped for a few minutes in
2
initially good but had gradually deteriorated in the past
the
traffic
three years. This culminated in his being asked to repeat
Total
19
his last class grade in school. The patient complained
about taunts from his peers in the school concerning his
*Scoring Scale
sleepiness. He was also unhappy about his uncontrolla-
0 =
would never doze, 1 = slight chance of dozing, 2 = moder-
ble
propensity to sleep. The patient is the second of
ate
chance of dozing
3 =
high chance of dozing
three children in a monogamous setting. His father is a
50
year old self-employed engineer and mother, a 43
year old unemployed university graduate. His siblings
were said to be doing well academically and there no
family history of hypersomnia or any mental disorder.
At
presentation he was well kempt, not pale, had no cer-
vical lymphadenopathy. His Body Mass Index (BMI)
A
B
C
was 22.1kg/m (Normal) while his Sexual Maturity Rate
2
Fig 1. (A) Axial cut showing normal cerebral mantle and ventricles. (B) Sagittal
and
(C) Coronal cuts showing mildly prominent sulci.

388
In
view of the indeterminate findings and duration of
present with depressive symptoms. Depression is often
debated as etiological or an outcome in hypersomnia.
3
sleep at night ( less than 10 hours) a clinical diagnosis of
hypersomnia of unknown etiology (idiopathic hyper-
Depressive symptoms have been noted in 15-25% of
patients with idiopathic hypersomnia. In our patient
3
somnia) without long sleep time, with complicating de-
pression, was made. The patient was commenced on
depression was considered as an outcome because of the
psychotherapy, oral amitriptyline (50mg b.i.d.) for de-
development of depressive symptoms after onset, and
pression and given clinic appointments to monitor his
with increasing severity, of EDS. The implication of
management. Depression and the confounding expres-
depression is particularly worrisome in the adolescent as
sion of suicidal ideation necessitated our prescription of
it
reduces adolescent productivity, increases the risk of
an
anti-depressant. The prescription of other effective
substance abuse and suicidality, and that of involvement
with the juvenile justice system.
20
anti-depressant drug such as fluoxetine, of the selective
serotonin re uptake inhibitors' class, was not considered
because of the history of suicidal ideation in the patient
The management of hypersomnia due to medical condi-
which itself is a side effect of the drug. Furthermore, the
tions focuses on the treatment of the etiological factors.
effectiveness of the use of a wake-promoting drug such
However there is currently no cure for idiopathic hyper-
somnia.
18,19
as
modanifil or that of a stimulant such as methyl pheni-
Its
contemporary scope of management in-
date
that has been demonstrated to provide variable suc-
clude the use of wake promoting medication such as
cesses in the treatment of idiopathic hypersomnia could
modanifil and stimulants such as methyl phenidateeven
not
be ascertained because the drugs are not available in
though they have been reported not to be very effective
our
practice.
3,18
He
was introduced to a series of absorb-
in
the management of idiopathic hypersomnia.
18,19
Be-
ing leisure time activities while counseling sessions
havioral approaches and sleep hygiene techniques have
were organized for him and other members of his fam-
also been employed with overall little beneficial ef-
fects. Spontaneous improvement in symptoms has been
19
ily. Informative interactive sessions were also under-
taken with his class teachers and school authority.
reported in a minority among a cohort of patients with
idiopathic hypersomnia.
18
The relative high cost of accessing health care for hyper-
Discussion
somnia in this study highlights the challenge that could
confront accessing health care for uncommon or com-
Hypersomnia of unknown etiology in this Nigerian ado-
plex health disorders in our environment with resultant
lescent was characterized by a seven year delay in diag-
defaults in management. This is even more remarkable
nosis, high cost of investigations and limited facilities
in
settings where there are no supportive or limited
for diagnosis of sleep disorders. Its impact included a
health care funds to access. Additionally, as it is with
most chronic disorders,
21
poor academic performance, depression, felt stigma,
hypersomnia could impact
suicidal ideation and increased family expenditure. Psy-
negatively on the physical, economic and psychosocial
cho social implications of hypersomnia have been re-
wellbeing of other family members.
ported from other regions of the world as well as the
Lack of facilities for conducting sleep studies and man-
dearth of facilities for sleep studies in the country.
1-3,7,8
agement of sleep disorders were limitations in the study.
It
took seven years and a significant progressive deterio-
The
weakness in the health systemís ability to provide
ration in academic in performance before a concerted
readily accessible and available services for sleep disor-
effort was undertaken by his caregivers to unravel the
ders, as observed in this study and other studies from the
country,
7,8
disorder. It underscores the poor degree of awareness
is
probably influenced by the health systems
about sleep disorders in the patientís immediate environ-
need
to address other more common childhood disor-
ment.
The perception of EDS as a form of laziness and
ders. Improving the health systemís capacity to manage
that
he will outgrow it further buttresses the assertion.
sleep disorder would enhance awareness, promote favor-
able
outcomes and strengthen health care delivery in
The
presentation of hypersomnia in adolescence could
general.
have
significant implications. It could reflect a past
1-4
history of head injury, encephalitis or, indicate the pres-
Hypersomnia was associated with diagnostic challenges
ence
of substance abuse. It could also signify the pres-
4
and
detrimental psycho social outcomes in this study.
ence
of a potentially ominous condition such as a brain
Improved awareness and a better outcome with hyper-
tumor. Furthermore, it could be indicative of more spe-
7
somnia, and other sleep disorders, could be achieved
cific sleep disorders such as narcolepsy, which is addi-
through communal enlightenment campaigns, instruc-
tionally characterized by cataplexy and hallucinations,
tional school health initiatives, provision of diagnostic
and Klein-Levin syndrome which has megaphagia and
facilities in the health system, training of teachers and
increased sexuality as complimenting features.
18,19
These
child health practitioners in the management of sleep
enumerated features that have been associated with hy-
disorders.
persomnia were absent in our patient. However he did

389
References
1.
El
Shakankiry HM. Sleep physiol-
9.
Orji I, Anyanwu OU, Ibekwe RC.
15.
Johns MW. A new method for
ogy
and sleep disorders in child-
Sleep hygiene of children in
measuring daytime sleepiness: the
hood. Nature
and Science
of Sleep
Abakiliki, South Eastern Nigeria.
Epworth Sleepiness Scale. Sleep
2011;3:101-14
Niger J Paediatr 2013; 40(3):322
1991;14 (6):540-5.
2.
Calhoun SL, Vgoontzas AN, Fer-
10.
Carskadon MA. Patterns of sleep
16.
Abiodun OA. A validity study of
nandez-Mendoza J, et
al . Preva-
and
sleepiness in adolescents. Pe-
the
hospital anxiety and depression
lence and risk factors of excessive
diatrician 1990;17:5-12
scale in general hospital units: a
daytime sleepiness in a community
11.
Li
S, Arguelles L, Jiang F, et
al .
community sample in Nigeria. Br J
sample of young children: the role
Sleep, school performance, and a
Psychiatry 1994; 165:669-72
of
obesity, asthma, anxiety/
school-based intervention among
17.
Giedd JN, Stockman M, Weddle
depression, and sleep. Sleep
school-aged children. A sleep se-
C, et
al . Anatomic Magnetic Reso-
2011;34(4):503-7
ries study in China. PLoS
One
nance Imaging of the Developing
3.
Dauvilliers Y, Lopez R, Ohayon
2013;8(7)e67928 doi: 10.1371/
Child and Adolescent Brain and
M,
Baynard S. Hypersomnia and
journal.pone.0067928
Effects of Genetic Variation.
Neu-
depressive symptoms: methodo-
12.
Millman RP. Excessive Sleepiness
ropsychology Review 2010;20(4):
logical and clinical aspects.
BMC
in
Adolescents and Young Adults:
349-61
M e d
2 0 1 3 ;
1 1 : 7 8
d o i :
Causes, Consequences, and Treat-
18.
Anderson KN, Pilsworth S, Shar-
10:1186/1741-7051-11-78
men
t
S
t r at egi e s.
P ed i at r
ples LD, Smith IE, Shneerson JM.
4.
Dauvilliers Y, Buguet A. Hyper-
2005;115;1774-86 DOI: 10.1542/
Idiopathic hypersomnia: a study of
somnia. Dialogues
ClinNeurosci
peds.2005-0772
77
cases. Sleep2007;30:1274Ė81
2005;7(4):347-56
13.
Owens JA. Sleep Medicine. In:
19.
Idiopathic hypersomnia- Wikipe-
5.
Full list of sleep disorders(ICSD-2)
Kliegman RM, Stanton BF, St.
dia, the free encyclopedia http://
- S
l e e p
J u
n k i e s .
h t
t p : / /
Geme J W, Schor N F,
Behrman
e n
. w i k i p e d i a . o r g / w i k i /
sleepjunkies.com/sleep-disorders/
RE,
editors. Nelson Textbook of
Idiopathic_hypersomnia[Last ac-
Pediatrics, 19
th
sleep-disorder-list-icsd-2/[Last
ed.
Philadelphia:
cessed 20/04/14]
accessed 18/04/14]
WB
Saunders Company; 2011. pp.
20.
Glied G, Pine DS. Consequences
6.
Ohayon MM. From wakefulness to
46-55.
and
correlates of Adolescent de-
excessive sleepiness:what we
14. LeBourgeois
M K,
Giannotti F,
pression. Arch
Pediatr Adolescent
know and still need to know.
Sleep
Cortesi F, Wolfson AR, Harsh J.
Med 2002; 156(10):1009-14
Med Rev 2008;12(2):129-41
The
relationship between reported
21.
Raina P, OíDonnell M,
7.
Ofovwe GE, Ofovwe CE, Okunola
sleep quality and sleep hygiene in
Rosenbaum P, et
al . The Health
P.
Prevalence and pattern of sleep
Italian and American Adolescents.
and
Well-Being of Caregivers of
disorder among
children with
Pediatr2005; 115(1):257-265 doi:
Children with Cerebral Palsy.
Pe-
neurological diseases in University
10.1542/peds.2004-0815H
diatr 2005;115(6):e626-36
of
Benin Teaching Hospital, Benin
City, Nigeria. Niger
J Paediatr
2012; 39(1):14-17
8.
Mume CO.
Excessive daytime
sleepiness among depressed pa-
tients. Libyan
J Med
2010; 5:
4626
DOI: 10.4176/091024